
Physician Assistants (PAs), also known as Physician Associates, play a critical role in the healthcare system, providing a broad range of services in various clinical settings. Similar to other advanced practice providers, scope of practice regulations for PAs can vary widely depending on the state in which they work.
Understanding state practice environments is essential for PAs to ensure compliance with local regulations and maximize their ability to care for patients. This guide provides an overview of the key factors that define state practice environments for Physician Assistants and how they impact the profession.
The Evolving Role of Physician Assistants
According to the American Academy of Physician Associates (AAPA), there are approximately 168,000 licensed physician assistants in the U.S., “engaging in more than 500 million patient interactions each year.”
The Physician Assistant profession has also experienced rapid growth in recent years. According to the National Commission on Certification of Physician Assistants (NCCPA), the number of Physician Assistants has grown by 76% over the past decade.
PAs have seen their roles evolve significantly over the years to become central figures in patient care. They now perform many of the same tasks as physicians, such as diagnosing illnesses, prescribing medication, and managing patient treatment plans. This evolution has necessitated a closer look at the regulatory frameworks that govern PA practice in various states.
Understanding State Practice Environments
A practice environment is essentially the governing state regulatory structure which determines a Physician Assistant’s scope of practice, or the extent to which they can practice autonomously.
Physician Assistants do not currently possess the same level of autonomy as Nurse Practitioners, and PAs are required to work with a collaborating physician in some capacity in almost every state. However, the level of required physician involvement can vary widely.
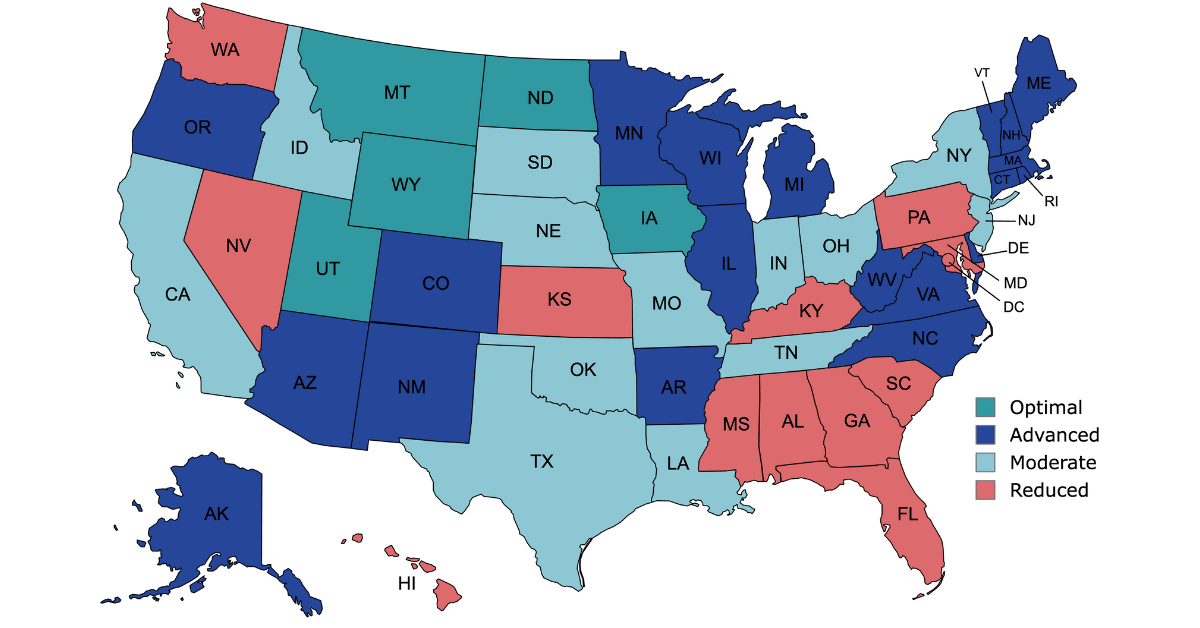
See the map below for a quick look at state practice environments for Physician Assistants.
Physician Assistant Scope of Practice Across the U.S.
Physician Assistant state practice environments are usually classified into four categories as defined by the AAPA: Optimal, Advanced, Moderate, and Reduced. Each category has implications for healthcare delivery, access, and PA autonomy.
The AAPA defines these four categories as follows:
“Optimal – PAs can practice to the full extent of their medical education, training, and experience. PAs continue to collaborate, consult, and/or refer to the appropriate member(s) of the healthcare team as indicated by the patient’s condition, the PA’s competencies, and the standard of care. The healthcare team, and/or their employer, may establish guidelines for collaboration, consultation, and/or referral beyond state laws and regulations.
Advanced – PAs practice to the full extent of their medical education, training, and experience, but must comply with additional administrative requirements as mandated in state law and/or regulation.
Moderate – State law and/or regulation requires additional administrative burdens that impact the practice environment. The PA and the healthcare team are limited in flexibility due to these administrative burdens.
Reduced – State law and/or regulation restrict the healthcare team and PAs’ ability to practice in at least one element of PA practice. Requires outdated practice models of limited delegated authority and/or restrictive supervision requirements.”
Source: American Academy of Physician Associates: “PA State Practice Environment”
Optimal Practice Environment
In Optimal practice environments, PAs enjoy the broadest scope of practice. These states typically grant PAs the authority to diagnose, treat, and prescribe medications independently, without mandatory supervision by physicians. Moreover, PAs in Optimal practice states often have prescriptive authority, enabling them to manage medications and controlled substances within established protocols.
There are currently five states that the AAPA grades as Optimal: Iowa, Montana, North Dakota, Utah, and Wyoming.
Advanced Practice Environment
Advanced practice environments impose some limitations on PAs compared to Optimal states, but still offer relatively unrestricted practice.
PAs in Advanced practice states may have limited prescribing privileges, necessitating physician co-signature or supervision for certain medications or procedures. While PAs in these states can perform a wide range of clinical duties independently, their scope of practice may be constrained in certain specialties or settings. Despite these limitations, Advanced practice environments afford PAs significant autonomy and professional development opportunities, enabling them to assume greater responsibility in patient care.
Moderate Practice Environment
Moderate practice environments strike a balance between autonomy and supervision for PAs, offering more flexibility than Reduced practice states but imposing greater restrictions than Optimal or Advanced practice jurisdictions.
While PAs may have prescribing authority, their autonomy is subject to physician oversight, particularly for complex medical conditions or treatments.
Reduced Practice Environment
In Reduced practice environments, PAs face the most stringent regulatory constraints, limiting their ability to practice independently or prescribe medications. These states often mandate direct physician supervision for all aspects of PA practice, including patient evaluations, treatment decisions, and prescription management.
PAs in Reduced practice states may have minimal autonomy and professional discretion, as their scope of practice is closely tied to physician directives.
Navigating Healthcare Compliance
Healthcare compliance is a significant concern for PAs, as it involves adhering to a myriad of regulations and laws at both the federal and state levels. These regulations are designed to protect patient safety, ensure quality of care, and maintain ethical standards in practice.
Understanding the collaboration requirements in your state is crucial for maintaining a positive working relationship with your collaborating physician and providing high-quality care to your patients. It also helps define the professional boundaries and responsibilities of each party, ensuring that patient care is delivered effectively and efficiently.
Collaborating Physician Requirements
One of the key areas of compliance for PAs is the requirement to have a collaborating physician. This relationship is governed by state laws and may include specific guidelines about the proximity of the physician, the frequency of communication between the PA and the physician, and the level of oversight required.
In some states, PAs and physicians must have a written agreement outlining the scope of practice and supervision requirements. In others, this agreement may not be necessary, but PAs must still work under the supervision of a physician. These agreements can be detailed, specifying the exact procedures a PA may perform, or they may be more general, providing overall guidelines for the PA-physician relationship.
Licensing, Certification, and Continuing Education Requirements
PAs must be licensed in the state where they practice and maintain national certification through the National Commission on Certification of Physician Assistants (NCCPA).
In addition, continuing education is a vital aspect of any healthcare profession, and PAs are no exception. Each state has its own continuing education requirements that PAs must meet to maintain their license and practice legally. This ongoing learning is necessary to keep pace with the rapidly evolving medical field and to ensure the highest standards of patient care. Keeping up with continuing medical education (CME) requirements and renewing licenses and certifications are important for compliance and professional development.

The Impact of State Regulations on Patient Care
State practice environments can have a profound impact on patient care. In states with more restrictive environments, PAs may be limited in their ability to provide timely and accessible care, especially in areas with physician shortages. On the other hand, states with full practice authority for PAs can expand access to healthcare services, particularly for underserved populations.
Addressing Healthcare Shortages
States that have embraced full practice authority for PAs are better positioned to address healthcare provider shortages. By allowing PAs to practice to the full extent of their abilities, these states can increase the healthcare workforce and improve access to care.
Improving Patient Outcomes
Research has shown that PAs can provide high-quality care with outcomes comparable to those of physicians. State regulations that enable PAs to practice independently can contribute to improved patient outcomes by facilitating a more collaborative and efficient healthcare team.
Best Practices for Navigating State Regulations
To navigate the complexities of state practice environments successfully, PAs should consider the following best practices:
Stay Informed
Regularly review state laws and regulations related to PA practice. You can do this by regularly checking your state’s medical board website or joining a professional organization, such as the AAPA, that provides updates on state regulations.
Additionally, attending conferences and networking with other PAs can provide valuable insights into regulatory trends and best practices.
Know Your Scope of Practice
Understanding your scope of practice is crucial for providing safe and effective care to your patients. Make sure you know what procedures and tasks you are authorized to perform under your state’s laws.
This knowledge not only ensures legal compliance but also empowers you to fully utilize your skills and training to benefit your patients.
Communicate with Your Collaborating Physician
Maintaining a positive working relationship with your collaborating physician can help you as a PA. Try to build a strong relationship, communicating openly and regularly with your physician to ensure you are both on the same page regarding your scope of practice and supervision requirements.
This dialogue helps prevent misunderstandings and fosters a team environment that is conducive to high-quality patient care.
Conclusion
Physician Assistants are vital to the healthcare system, and understanding state practice environments is crucial for their practice. While variations in state laws can pose challenges, they also offer opportunities for PAs to advocate for change and improve healthcare access for patients. By staying informed, building collaborative relationships, and continuing professional development, PAs can navigate these environments effectively.
In summary, state practice environments for Physician Assistants are shifting landscapes that require vigilance, adaptability, and active participation from PAs. As healthcare continues to evolve, so too will the roles and regulations surrounding this profession.
Don’t Navigate Regulations Alone – Get Started with Zivian Health
Zivian Health was created to handle all the challenges of healthcare compliance so that you can stay focused on providing care.
If you are seeking a collaborating physician or support with regulations, contact our team today!